A Comprehensive Guide to Medicaid and Wound Care Supply Coverage

Does Medicaid cover wound care supplies? Yes, most state Medicaid plans do cover wound care supplies, but the type and extent of coverage can vary significantly from state to state. If you're eligible for Medicaid, it's important to verify the specifics of your coverage.
Wound care is an essential part of recovery for many, especially those with chronic conditions or recovering from surgery. Adequate supplies—like dressings and gauze—are crucial for preventing infection and promoting healing. However, accessing and affording these supplies can be a major concern for many individuals, particularly those on limited incomes.
Understanding what Medicaid covers in terms of wound care supplies is vital for anyone who relies on these essential products for their health and healing. Here, we aim to clarify these details, streamline the process of gaining access to necessary supplies, and ensure that you can focus more on healing and less on the logistics of healthcare coverage.

Understanding Medicaid Coverage for Wound Care Supplies
Navigating Medicaid and its coverage for wound care supplies can be confusing, but it's crucial to understand how you can access the supplies you need for proper wound care management. Here’s a straightforward guide to help you grasp the essentials of does Medicaid cover wound care supplies, eligibility criteria, state variations, and what exactly is covered.
Eligibility for Medicaid Coverage of Wound Care Supplies
To be eligible for wound care supplies coverage under Medicaid, you must first be enrolled in Medicaid, which typically serves low-income individuals and families. Eligibility can also depend on specific health conditions that require such supplies for treatment. It’s important to consult with your healthcare provider to determine if your condition qualifies under Medicaid’s guidelines.
State Variations in Coverage
Medicaid is administered at the state level, which means coverage for wound care supplies can vary significantly from one state to another. While most states provide coverage for basic wound care supplies, the extent and type of covered items can differ. For example, some states might cover advanced wound dressings under certain conditions, while others may only cover the basics such as gauze and tape. It's essential to contact your local Medicaid office to understand the specifics of what is covered in your state.
Covered Items
Generally, Medicaid covers a range of wound care supplies deemed medically necessary. These typically include:
- Primary Dressings: Such as foams, alginates, hydrocolloids, and hydrogels that directly contact the wound.
- Secondary Supplies: Including bandages and tapes used to hold primary dressings in place.
- Disposable Supplies: Such as wipes and gloves to ensure a sterile environment during wound care.
- Durable Medical Equipment (DME): In some cases, items like compression pumps and specialized beds for pressure ulcer prevention are covered.
It is important to have a prescription or a documented recommendation from a healthcare provider to ensure that these supplies are covered under Medicaid. The documentation should clearly state the medical necessity of the supplies for your specific wound care needs.
ProMed DME stands ready to assist you in navigating these complexities by providing detailed information on Medicaid coverage in your state and helping you access the necessary wound care supplies. By understanding the types of supplies covered and ensuring you meet the eligibility criteria, you can better manage your wound care effectively and reduce out-of-pocket expenses.
By familiarizing yourself with the details provided here, you can take proactive steps towards managing your health care needs more efficiently. Effective wound care is not just about treatment—it's about accessing the right supplies without undue financial burden.
Types of Wound Care Supplies Covered by Medicaid
When it comes to wound care, having the right supplies is crucial for proper healing. Does Medicaid cover wound care supplies? Yes, Medicaid generally covers a variety of wound care supplies, but the specific types and coverage can vary by state. Here’s a breakdown of the common categories of supplies that are often covered:
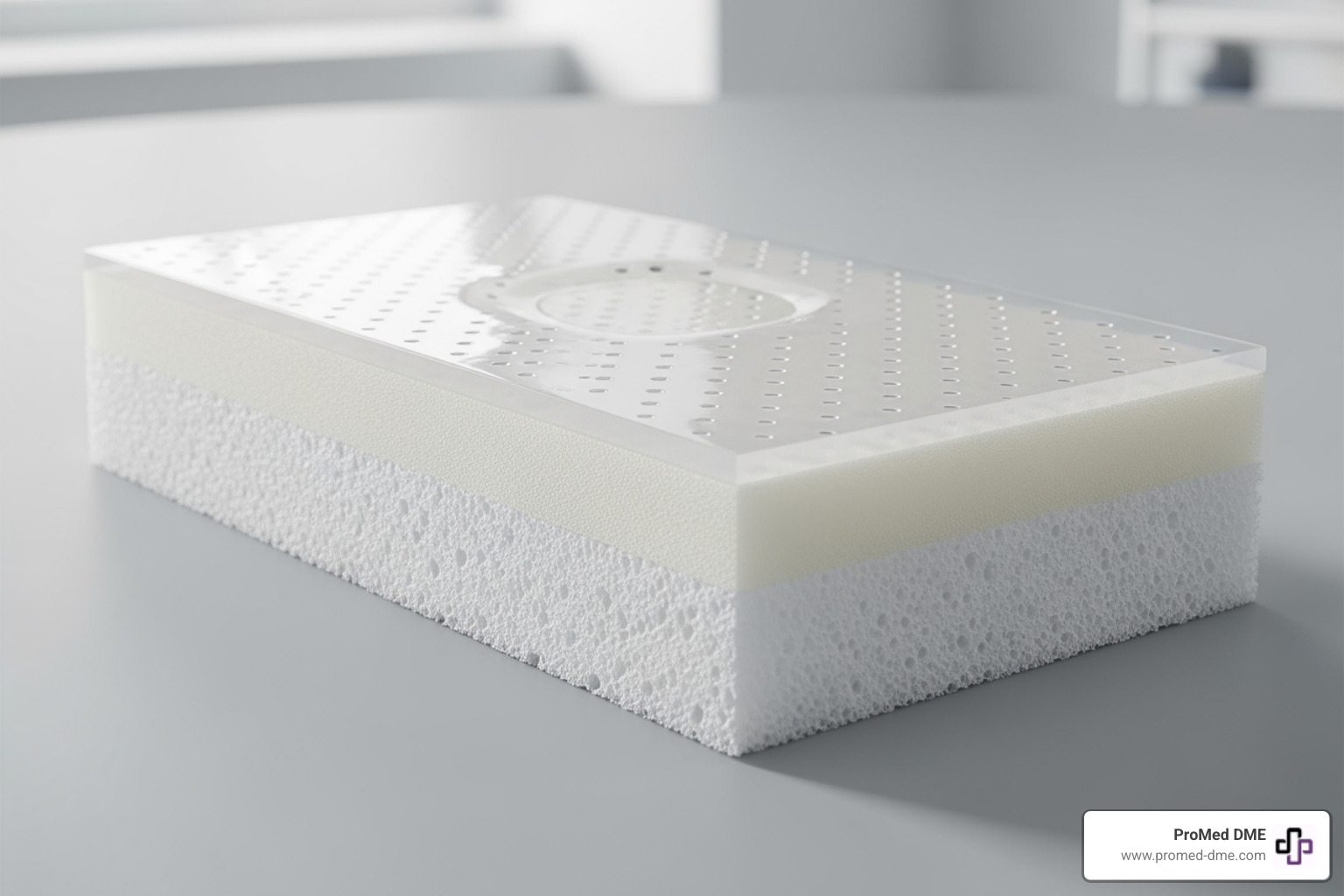
Primary Dressings
Primary dressings are materials that come in direct contact with the wound. Medicaid typically covers these as they are essential for the treatment of wounds. Common types of primary dressings covered include:- Sterile gauze pads: Used for absorbing wound exudate and protecting the wound from infection.- Hydrogel dressings: Maintain a moist environment and help with pain relief.- Hydrocolloid dressings: Promote healing in dry wounds by creating a moist environment.- Alginate dressings: Highly absorbent and ideal for wounds with significant drainage.
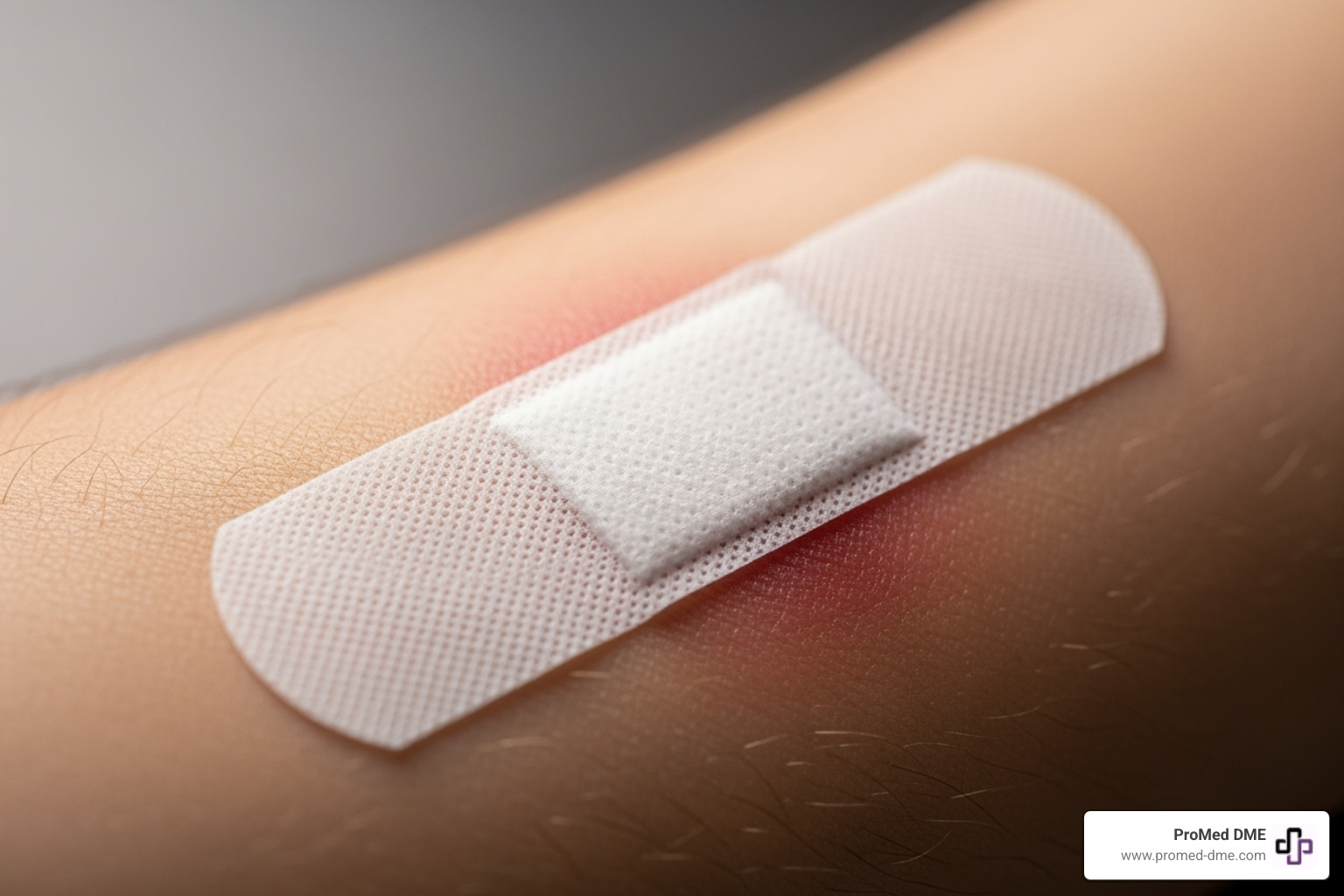
Secondary Supplies
Secondary supplies are used to secure primary dressings and further protect the wound. These include:- Bandages: Used to hold dressings in place and provide additional protection and compression.- Adhesive tapes: Secure bandages and dressings without restricting movement.- Gauze: Acts as a secondary absorbent layer, often used in wrapping and securing wound dressings.
Disposable Supplies
While some disposable supplies are essential, Medicaid coverage for these can be limited. Typically, everyday items like:- Adhesive bandages (e.g., Band-Aids)- Topical antibacterial creamsare not covered as they are considered general-use items rather than specific wound care treatments.
Durable Medical Equipment (DME)
For more severe or long-term wound care needs, Durable Medical Equipment may be necessary and is often covered under Medicaid. This includes:- Pressure mattresses: Help prevent and manage pressure ulcers.- Wound vacuums: Assist in the healing of more complex wounds by reducing air pressure around the wound.
Special Considerations
While Medicaid covers many types of wound care supplies, the approval for coverage requires that the items are deemed medically necessary by a healthcare provider. This means the supplies must be prescribed by a physician or a qualified healthcare provider to be eligible for coverage.

Understanding the types of wound care supplies covered by Medicaid allows you to better prepare for managing your wound care regimen. Always check with your state's Medicaid program for the most accurate and detailed information on coverage to ensure you receive the necessary supplies while minimizing out-of-pocket costs.
How to Access Wound Care Supplies Through Medicaid
Accessing wound care supplies through Medicaid involves a straightforward process, though it varies slightly from state to state. Here's a step-by-step guide to help you navigate the enrollment process, understand provider prescriptions, and utilize direct billing with ProMed DME.
Enrollment Process
To access Medicaid-covered wound care supplies, you first need to be enrolled in Medicaid. If you're not already enrolled, you can apply through your state's Medicaid agency. Once enrolled, you'll receive a Medicaid card and a list of approved providers, including those who supply wound care products.
Provider Prescriptions
Before Medicaid approves coverage for wound care supplies, a healthcare provider must declare these items as medically necessary. This means you need a prescription from your doctor or a qualified healthcare provider. The prescription should detail:
- The type of wound
- The specific supplies needed
- The quantity and frequency of supply use
It's important to keep this prescription updated and to have regular check-ups to adjust the prescription as your wound care needs change.
Direct Billing
With a valid prescription, you can directly order your wound care supplies from approved suppliers who bill Medicaid directly. This eliminates the need for upfront payments and subsequent reimbursements, simplifying the process.
ProMed DME stands out as a convenient option here. We coordinate directly with your healthcare provider to ensure all paperwork and prescriptions are in order. We then directly bill Medicaid on your behalf, ensuring a seamless supply of the necessary wound care products right to your doorstep.
By following these steps and utilizing services like ProMed DME, accessing your necessary wound care supplies through Medicaid can be an efficient and stress-free process. This ensures you focus more on healing and less on the logistics of healthcare supply management.
Navigating the Billing and Reimbursement Process
Navigating the billing and reimbursement process for Medicaid-covered wound care supplies doesn't have to be complicated. Here's a straightforward guide to help you understand and manage this process effectively.
CPT Codes
CPT codes, or Current Procedural Terminology codes, are crucial for billing. These codes tell Medicaid what kind of care was provided. For wound care supplies, specific CPT codes correspond to different types of dressings and treatments. For example, codes like A6021 (for gauze) or A6203 (for composite dressings) specify the type of supply used. It's important that these codes are accurate to avoid delays in reimbursement.
Documentation
Documentation is the backbone of the reimbursement process. You need detailed records that include:- The prescription from your healthcare provider.- A detailed description of the wound and the necessary treatment.- Records of any previous wound care treatments and outcomes.
This documentation proves that the wound care supplies are medically necessary, which is a requirement for Medicaid coverage.
Claim Submission
Submitting a claim involves several steps:1. Gather all necessary documentation: This includes medical records, a list of supplies used (with corresponding CPT codes), and the Medicaid coverage confirmation.2. Fill out the claim form: Ensure all sections are completed accurately. Any error can result in a delay or denial of the claim.3. Submit the claim to Medicaid: This can typically be done electronically through a billing system or via mail if required.
ProMed DME handles this process for you, submitting all necessary paperwork and claims to ensure you receive your supplies without any hassle.
Reimbursement Rates
Reimbursement rates can vary based on the state and the specific Medicaid plan. These rates are predetermined and are meant to cover the cost of the supplies and any associated services. Understanding these rates can help you anticipate any potential out-of-pocket costs, although with Medicaid, these are typically minimal or non-existent for covered supplies.
By understanding these key components, you can navigate the billing and reimbursement process more confidently. With providers like ProMed DME, much of this process is managed for you, allowing you to focus on recovery and management of your health. This streamlined approach ensures that you receive the necessary wound care supplies timely and efficiently, reducing any potential stress associated with billing and insurance claims.
Enhancing Wound Care at Home with Medicaid-Covered Supplies
When managing wound care at home, having the right supplies and support is crucial for effective healing and comfort. Medicaid coverage can significantly enhance your home care regimen by providing necessary supplies and additional services. Here’s how you can make the most of your Medicaid benefits for wound care at home:
Home Safety Modifications
To prevent injuries and make home care more manageable, Medicaid may cover various home safety modifications. These adjustments can include installing grab bars, ramps, and widened doorways to accommodate mobility aids. Such modifications ensure that your living environment supports your recovery and daily needs.
At-Home Food Delivery
Proper nutrition is vital for wound healing. Medicaid may cover at-home food delivery services, providing nutritious meals that meet your dietary needs without the need for grocery shopping or meal preparation. This service is especially beneficial for individuals with limited mobility or those who cannot cook for themselves.
Medical Supply Deliveries
Does Medicaid cover wound care supplies? Yes, and getting these supplies is made easier with services like ProMed DME. They can deliver essential wound care products directly to your home, such as sterile gauze, antiseptic wipes, and appropriate dressings. This convenience ensures you always have the necessary supplies on hand, without the hassle of visiting a pharmacy or store.
Self-Care Tips
Alongside using the right supplies, proper wound care involves adhering to best practices for wound management. Keep the wound clean and dry, change dressings as recommended by your healthcare provider, and monitor for signs of infection such as increased redness, swelling, or pain. Medicaid may also cover consultations with healthcare professionals who can provide personalized advice and guidance.
By utilizing these Medicaid-covered services and supplies, you can enhance your wound care routine at home, promoting faster healing and greater comfort. Always ensure to consult with your healthcare provider to understand the full extent of benefits available to you under your specific Medicaid plan.
Frequently Asked Questions about Medicaid and Wound Care Supplies
Does Medicaid cover negative-pressure wound therapy?
Yes, Medicaid covers negative-pressure wound therapy (NPWT) when it is deemed medically necessary and prescribed by a healthcare provider. This therapy uses a vacuum dressing to promote healing in acute or chronic wounds and is commonly used for serious wounds that are not healing well with standard treatments. However, coverage can vary by state, so it’s important to check with your local Medicaid office or a ProMed DME specialist to understand your specific benefits.
How often can I receive new wound care supplies through Medicaid?
Medicaid typically allows for the regular replacement of wound care supplies based on the medical necessity and as prescribed by your healthcare provider. For most wound dressings and supplies, a new order is required every 3 months. However, the frequency can increase if there's a change in the dressing type or if the quantity needed changes. Always ensure that your prescriptions are up-to-date and that your healthcare provider has documented the necessity for frequent changes in your medical records.
Are there any wound care supplies Medicaid does not cover?
While Medicaid covers a broad range of wound care supplies, there are some exceptions. Supplies that are considered non-essential or not directly related to wound healing, such as certain types of cleansers or moisturizers that are not specific to wound care, may not be covered. Additionally, items that are deemed as convenience items rather than medical necessities are typically not covered. It's crucial to consult with a Medicaid representative or a ProMed DME product specialist to confirm whether a specific item is covered under your plan.
By understanding these key points, you can better navigate the coverage provided by Medicaid for wound care supplies, ensuring you receive the necessary treatments without undue financial burden. Clear communication with your healthcare provider and Medicaid is essential to optimize your use of covered wound care supplies.
Conclusion
At ProMed DME, we understand that navigating Medicaid coverage for wound care supplies can be complex. That's why we're committed to assisting you every step of the way. Our goal is to ensure that you have access to the essential wound care products you need without the stress of handling intricate insurance details.
Does Medicaid cover wound care supplies? Yes, most Medicaid plans do, but understanding the specifics of what is covered and how to access these benefits can make a significant difference in your healthcare experience. Our team at ProMed DME specializes in providing high-quality wound care supplies that are often covered by Medicaid. We pride ourselves on our ability to simplify the process, from selecting the right products to handling insurance paperwork.
We encourage you to explore our comprehensive range of wound care products on our wound care page. Here, you will find everything from basic gauze and bandages to advanced dressing materials. Our knowledgeable staff is always ready to provide guidance on product selection based on your specific medical needs and Medicaid coverage.
Effective wound care is crucial for healing and recovery. With ProMed DME, you can be confident that you're getting not only the supplies you need but also the support necessary to use them effectively. We are here to help you improve your health and wellbeing with quality care and comprehensive service.
For any questions about product options, Medicaid coverage, or to start an order, please do not hesitate to contact us. Our team is dedicated to providing you with the best possible service and ensuring your medical supply needs are met with ease and efficiency. Let ProMed DME be your trusted partner in managing your wound care and enhancing your overall quality of life.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.